Hadassah: New Software Tells Brain Surgeons Where to Cut
At Jerusalem’s Hadassah Hospital, a team of neurosurgeons and computer scientists are developing software to plan the delicate incisions that are necessary for neurosurgery. “Field of image or computer-assisted surgery is a very evolving project in medicine—especially in neurosurgery,” says Dr. Yigal Shoshan, head of Hadassah Hospital’s neurosurgery department, who along with Leo Joskowicz, a Hebrew University computer science professor, is developing the software.
Typically, a doctor plans for surgery by looking at an MRI brain scan and, using his or her own knowledge and experience, chooses the best locations to cut. When Dr. Shoshan, now 56, was a young resident 30 years ago, he didn’t have the luxury of computer printouts. He based his decision on his knowledge of anatomy and what he saw in anatomy textbooks. “Today it is very different. We are using technology to help us localize very precise areas in the brain and to preserve functions of the brain that are very important,” he says.
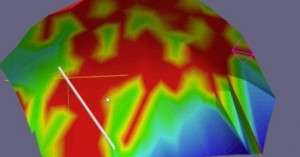
The software combines a wide array of data to create a 3-D brain map instead of the traditional two-dimensional MRI. Functional MRIs capture blood flow changes that reflect areas of heightened neural activity, rather than simply an image of the organ. Overlaying the functional MRI image is another data set from a Magnetic Resonance Angiography (MRA), which focuses on the brain’s arteries and highlights irregularities, blockages and aneurysms.
All this data is processed to generate green and red color codes representing where surgeons should and should not cut. The areas that the software analyzes as too dangerous or too close to vital parts of the brain are placed in the red zone. Not only does it allow for safer surgeries, it potentially paves the way for more effective treatment. “If we are inserting an electrode to the basal ganglia of the brain to treat Parkinson’s—we are talking about sub-millimetric accuracy,” he says.
Last summer, a team of six scientists and computer engineers tested their prototype at Hadassah Hospital. In one test case, they gave the doctors a basic MRI showing a lesion on it. They asked each of the 10 doctors to plan a surgery based on the MRI alone, and then compare their plan with the software’s suggestions. Altogether, their experiment analyzed more than 240 surgical paths.
While the final results of the study have yet to be published and the software has yet to get FDA approval for further testing, Dr. Shoshan says the results would show how the software enables doctors to pick more accurate and safer trajectories.
Image: Color-coded head surface model presenting the risk ratio for a given surgical trajectory. Red is analyzed to be a no-go surgical area and green means a lower-risk surgical incision area. Courtesy Dr. Yigal Shoshan.