A quick guide for the patients
What is called a hernia?
A hernia (or herniation) is defined a defect or opening on the abdominal wall. Hernia may be congenital (defect since birth) or acquired (develops due to weakness of the wall or after injury). Hernias are very common, affecting 10-15% of population and may involve equally men and women.
How do you recognize a hernia?
Hernias most commonly present as a visible protrusion or lump, as a result from the projection of an intra-abdominal organ (usually intestine or fat) through the abdominal wall opening, creating a defect on the surface of the skin.
Hernias may present with pain or inconvenience, commonly aggravated with exertion. On the other hand there may be present without any symptoms at all. In worst cases, hernias may cause severe pain due to injury to abdominal viscera, or even intestinal obstruction (incarcerated hernias). In this case, the patient must be operated as soon as possible or else the danger of intestinal necrosis is imminent!!!
What are the symptoms of hernias?
• Visible lump under the skin
• Pain associated with exertion or weight lifting
• Inconvenience or pain during walking or jogging
What to expect when you have a hernia?
Generally with time, hernias have the tendency to grow in size, while the symptoms usually worsen. A surgical repair is the exclusive treatment for hernias.
What are the causes of hernias?
• Previous surgical operations
o The surgical incisions commonly weaken the abdominal wall, allowing hernia formation.
• A rapid increase in the size of the abdomen
o Rapid weight gain
o Pregnancy
• Prolonged increase of the intrabdominal pressure
o Weight lifting
o Chronic cough
o Constipation
o Disturbances in urination (prostate gland hypertrophy in men)
Why should we repair a hernia?
The only permanent treatment of hernia is the surgical repair. Patients with hernias are in danger of developing serious complications including entrapment and tightening of intestine (incarceration) which may subsequently cause intestinal obstruction and ischemia (disturbances of the intestinal blood flow may lead to gangrene). Both these conditions demand urgent surgical treatment.
The scheduled (non-urgent) surgical correction of hernia generally has better clinical results, shorter recovery and significantly less post-operative complications.
Signs indicating possible hernia incarceration
• Intense abdominal pain or abdominal distension
• Nausea and vomiting
• Redness, sensitivity or pain at the location of skin lump
Which are the most common types of hernias?
• Inguinal hernia – Scrotal-inguinal hernia
• Femoral hernia
• Omphalocele
• Epigastric hernia
• Postsurgical abdominal hernia – over previous surgical incisions.
• Sports hernia
• Less common forms (Spiegel’s hernia, Richter’s hernia, Littré’s hernia, lumbar hernia, obturator hernia etc.)
Inguinal hernias are by far the commonest type of hernias!
A hernia may present in 10% of post-surgical incisions.
How does a hernia appear?
Which are the treatment options for a hernia?
• Surgical treatment:
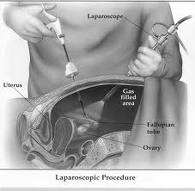
– Laparoscopy – Performed through minimal skin incision with the use of HighDefinition (1080p) camera and special laparoscopic equipment.
– Robotic – The robotic technology allows supreme quality of image to the surgeon (3-dimensional– HighDefinition 1080p) and comfort maneuvering in narrow spaces, using special Endowrist Instruments. It is considered the best approach for the treatment of abdominal hernia.
– Open surgery – Repair through larger skin incision with conventional means.
• Conservative treatment: The use of trusses or bandages should be avoided. Long term use may cause adhesions in the area or injury to the intestine.
Hernia Treatment – Laparoscopic surgical repair
Laparoscopic hernia repair has become very popular over the past 20 years. For many surgeons the laparoscopy has become the main surgical approach for hernia repair. The advantages of laparoscopy include the following:
• Bloodless
• Minimal post-operative pain
• Swift recovery
• Quick return to everyday life and to occupation
• Excellent cosmetic result
The laparoscopic repair for inguinal hernia, how is it performed?

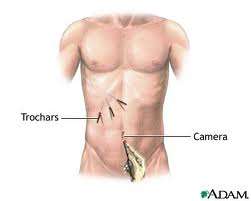
The operation is performed through 3 small skin incisions, one of which is 8mm wide, under the umbilicus from which the optic laparoscope is inserted, while each of the other two is 5mm wide along the midline of lower abdomen, through which laparoscopic instruments are inserted. The optic laparoscope is connected to high definition monitors. With microsurgical technique the hernia is corrected and the abdominal wall is strengthened with a mesh. The mesh (10x16cm) is made of non absorbable material and it is perfectly compatible with the body tissues.
We use the Extraperitoneal technique (TEP – Totally ExtraPeritoneal repair) which is currently regarded as the safest method for inguinal hernia repair. This technique is being used in our department since 1991 with a recurrence ratio less than 0.5%. The personal experience is considered among the greatest in a worldwide level for a single surgeon, exceeds a number of 3.000 operations of this kind.
What is the laparoscope?
Laparoscope is a long slim telescope that allows the surgeons to visualize and examine parts of the abdomen (laparoscopy comes from the Greek lapara=abdomen). Furthermore, the laparoscope is connected to a video camera and the image is transferred to a monitor. This technology allows visualization of the surgical field in high definition monitors and conduction of the operation through very small (a few millimeters) skin incisions.
What types of laparoscopic inguinal hernia correction exist?
There are two different types widely used:

1. TransAbdominal Properitoneal Procedure (TAPP): This technique involves entering the abdomen (where the viscera is located), opening the peritoneal membrane (abdominal lining) from inside, restoring the anatomy in the region of hernia, placing the mesh to strengthen the wall and finally closing the peritoneum over the mesh.
2. Totally ExtraPeritoneal repair (TEP): In this technique we do not enter the abdomen (peritoneal cavity). The whole procedure is performed within the layers of the abdominal wall (properitoneal layer). The hernia is identified and corrected, and subsequently the mesh is inserted within to strengthen the abdominal wall.
Which laparoscopic technique is better?
Surgeons have different preferences among the available laparoscopic techniques for inguinal hernia repair. In expert hands, both techniques have excellent results. Our team, although initially has used the TAPP technique, since 1993 is being using the extraperitoneal (TEP) method for avoiding entrance into the peritoneal cavity.
What are the advantages of the laparoscopic technique?

The laparoscopic technique requires smaller incisions without causing injuries to the muscles. This causes less postoperative pain and faster recovery.
The laparoscopic image is magnified, facilitating proper recognition of testicular vessels and nerves in man, hence preventing any damage. The laparoscopic technique is ideal for the management of bilateral inguinal hernia, where both sides can be equally be repaired from the same midline incisions. Also the laparoscopic repair is the treatment of choice for recurrent inguinal hernias after previous open surgical procedures.
Is every patient with inguinal hernia suitable for laparoscopic intervention?
The answer is yes, with only very few exceptions.
What does the preoperative preparation involves?
• You’d better avoid having dinner or drinking fluids after midnight, the night before surgery.
• You may have a shower the day before or early in the morning of the operation.
• The use of laxative lies on the preference of your surgeon.
• Depending on your age and the type of anesthesia, some examinations may be necessary prior to operation, such as :
• Blood count and blood coagulation tests
• ECG and cardiologic evaluation
• Chest X ray
What is the preparation prior to laparoscopic surgery?
• In most cases of laparoscopic hernia repair, one day hospitalization is needed.
• In many instances, patient may be discharged the same day with surgery.
• Do not shave the area near the hernia (this might increase the possibility of infection). If needed the surgical team will prepare the skin just before surgery.
• Avoid or stop medication such as aspirin, anti-coagulants or anti-inflammatory agents, 7-10 days prior to surgery.
• Inform your doctor about all medication you receive.
What possible complications are related to laparoscopic surgery for inguinal hernia?
• Rarely, the possibility of bleeding, wound infection and even mesh infection is possible.
• Even less frequent are injuries to the organs of the inguinal region.
• Hernia recurrency.
Is possible the conversion of laparoscopy to open surgery?
No, it is unlikely that this might happen. However, for some patients and for specific reasons it might be necessary to convert surgery to open. The conversion of the laparoscopy to the traditional open technique is not considered a surgical complication.
What to expect from laparocopic hernia repair?
• You will be discharged as soon as you will be able to drink fluids, stand up on your feet and urinate.
• You may return to everyday activities within a couple of days.
• Even though you may feel well right after surgery, we recommend our patients to rest for a few days.
• For full recovery usually 1-2 weeks are needed.
• Regardless of how well you may feel post-operatively, you should better be re-examined by your surgeon within one week from surgery.
How can I reduce the possibility of recurrence?
We recommend avoiding of aggravating factors such as heavy weight lifting, intense exercise of the region and increased intrabdominal pressure during the early post-operative period. Make sure that you inform your doctor before returning to any activity of this kind.


Other considerations and measures include:
• Avoiding prolonged constipation (fiber-rich diet)
• Reduce of chronic cough (cut off smoking)
• Reduce micturition difficulties (prostate gland examination in men)
• Proper exercise that does not strain lower abdominal muscles.